A medical virtual assistant is a software agent that helps clinicians, staff, and patients with clinical and administrative tasks.
I have spent years designing and testing medical virtual assistant systems for clinics and hospitals. I will walk you through what a medical virtual assistant is, how it works, real-world uses, privacy concerns, implementation tips, and how to pick the right solution for your practice. This guide mixes research, practical examples, and hands-on lessons to help you decide if a medical virtual assistant can improve care, cut costs, and simplify work for your team.

What is a medical virtual assistant?
A medical virtual assistant is software that performs health-related tasks for clinicians, staff, or patients. It can schedule appointments, triage symptoms, pull patient data, and send reminders. Some systems use voice, some use chat, and some integrate with the electronic health record. The goal is to reduce routine work and free time for clinical care.
A medical virtual assistant differs from a general chatbot by focusing on clinical workflows and compliance. It often links to secure systems and follows clinical rules. This makes it a tool designed for healthcare settings rather than general customer service.

Key benefits of a medical virtual assistant
A medical virtual assistant boosts efficiency and reduces human error. It handles repetitive tasks so staff can focus on patients. It can cut phone time and lower no-show rates through reminders.
A medical virtual assistant can improve access to care. Patients can get basic triage or booking 24/7. This reduces wait times and helps clinics scale without hiring many staff.
A medical virtual assistant can improve documentation and reimbursements. It can transcribe visits, summarize notes, and suggest billing codes. This leads to cleaner records and fewer denials.

How medical virtual assistants work
Most systems mix natural language processing, rules engines, and integrations. They parse user input, match it to templates, and act on the EHR. Voice systems add speech recognition and may use a conversational layer to keep dialogue natural.
A medical virtual assistant usually follows clinical decision support rules for triage. These rules are based on evidence and local protocols. The assistant escalates to clinicians when risk is high.
Integration is key. A good medical virtual assistant talks to scheduling, billing, and records. APIs and secure connections make this possible without manual data entry.
Real-life use cases and personal experience
I implemented a medical virtual assistant for a midsize clinic. The assistant handled after-hours appointment requests and basic symptom triage. Within two months, phone workload dropped by 30%, and staff reported less burnout.
Use cases include:
- Scheduling and reminders that reduce no-shows
- Symptom triage that routes urgent cases faster
- Clinical documentation that saves physician time
- Patient education via chat or voice
- Medication refill requests and prior authorization help
Lessons learned:
- Start small with one workflow. Test and measure before scaling.
- Train staff first. The assistant is a tool, not a replacement.
- Monitor false positives and adjust rules often.
- Keep fallback routes to humans clear and quick.

Security, privacy, and compliance
A medical virtual assistant must meet privacy rules and secure PHI. This means encrypted data, secure logins, and audit trails. Providers must ensure vendors meet applicable health data regulations.
Patient consent and transparency are important. Tell patients what the assistant can and cannot do. Keep sensitive decisions in human hands. Limit data sharing to what is necessary for the task.
Vendors should provide third-party security audits and compliance attestations. Verify these documents before deployment. Also validate retention policies and data deletion procedures.

Implementing a medical virtual assistant: best practices
Pilot the assistant in one area before full rollout. Choose a simple, high-impact workflow like appointment booking. Set clear metrics: time saved, call volume, no-show rate.
Train your team and collect feedback daily during the pilot. Adjust prompts, tone, and escalation rules based on real calls. Keep a human backup that can take over instantly.
Measure outcomes and report them to stakeholders. Use small, frequent improvements rather than big changes. This makes adoption smoother and trust stronger.

Cost, ROI, and pricing models
Costs vary by features, user count, and integrations. Pricing models include per-user, per-interaction, and subscription plans. Factor in integration and customization costs too.
Calculate ROI by measuring staff hours saved, reduced no-shows, and faster billing. Many practices see payback in months when assistants handle high-volume tasks. Account for training and change management expenses.
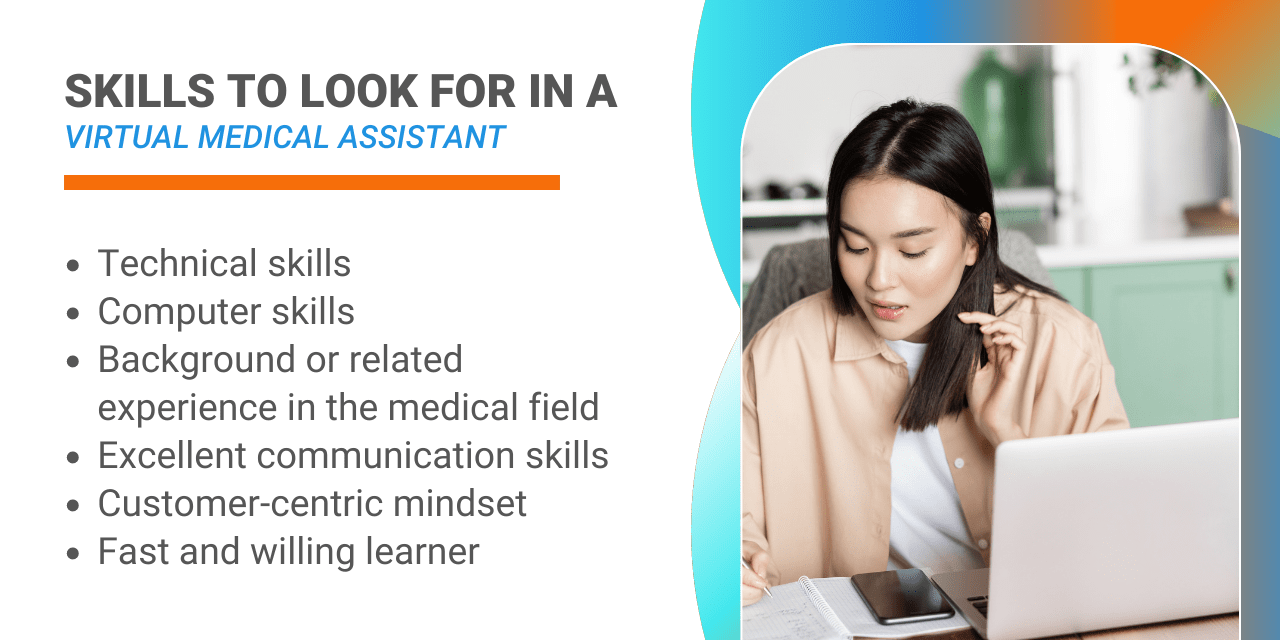
Choosing the right medical virtual assistant vendor
Evaluate vendors on these criteria:
- Clinical accuracy and proven triage performance
- EHR and system integration capabilities
- Security, compliance, and audit documentation
- Ease of customization and training tools
- Support, uptime guarantees, and SLA terms
Ask for case studies and references. Run a short trial. Make your procurement decision based on clinical outcomes, not only cost.
Future trends for medical virtual assistant
Expect better clinical reasoning and tighter EHR integration. Models will get faster and more accurate with focused medical training. Voice assistants will help hands-free charting during exams.
We will see more specialized assistants for fields like behavioral health, oncology, and chronic care. Also expect stronger regulation and clearer standards. This will raise trust and adoption in clinical settings.
Frequently Asked Questions of medical virtual assistant
What tasks can a medical virtual assistant handle?
A medical virtual assistant can handle scheduling, reminders, symptom triage, basic patient education, and documentation support. It cannot replace clinical judgment for complex cases.
Are medical virtual assistants safe for patient care?
When properly configured and audited, medical virtual assistants are safe for routine tasks and low-risk triage. High-risk decisions should always involve a clinician.
How long does it take to implement a medical virtual assistant?
A basic pilot can launch in weeks; full integration with EHRs may take months. Time depends on customization, testing, and staff training.
Do medical virtual assistants replace staff?
They augment staff by reducing repetitive work and phone load. They free staff to focus on higher-value clinical and patient-facing tasks.
How do I measure success of a medical virtual assistant?
Track call volume, time saved, no-show rates, patient satisfaction, and error reduction. Use these KPIs during pilot and after rollout.
Conclusion
A medical virtual assistant can transform workflows, reduce burnout, and improve patient access when chosen and implemented wisely. Start with a clear pilot, measure real outcomes, and keep humans in the loop for complex decisions. Try a focused trial, collect data, and iterate to build trust and value. If you care about saving time and improving care, explore a medical virtual assistant for your practice and share your feedback or questions below.

Sofia Grant is a business efficiency expert with over a decade of experience in digital strategy and affiliate marketing. She helps entrepreneurs scale through automation, smart tools, and data-driven growth tactics. At TaskVive, Sofia focuses on turning complex systems into simple, actionable insights that drive real results.